A novel reconstructive surgery for lower eyelid defects
Skin cancer rates in Aotearoa are among the highest in the world, leading to more frequent recurrences and increased surgical interventions. This has significant clinical implications in ophthalmology, particularly in oculoplastics, where the management of eyelid tumours poses both functional and aesthetic challenges.
Full-thickness lower eyelid defects following tumour excision present a substantial reconstructive dilemma due to the complex anatomy and its impact on eye health and vision. Traditional reconstructive techniques cover such defects by making use of healthy tissue harvested from the lateral canthus (eg. Tenzel flap), the upper lid (eg. Hughes flap) or other places (eg. the nasal septum or the ear). These options, nonetheless, sacrifice healthy tissue which could be extremely useful in cases of recurrence or new tumours in the same area, creating a challenging iatrogenic morbidity.
Some of these traditional procedures cause severe disruption in patients' lives, requiring a two-step surgery where the eye remains closed for a few weeks between the first and second operation.
MARCH technique
The need for a minimally aggressive procedure to avoid these significant problems spurred the development of a novel reconstructive procedure: the Marginal Approach for Releasing the Lid with Closure Handling (MARCH) technique1. This procedure can serve as a first-line single-step reconstruction for central and medial lower eyelid full-thickness defects of up to almost 80%. The principle of this technique is based on using the remnant lateral lower eyelid for the whole defect reconstruction by separately mobilising the two lamellae. It follows two basic steps: the release of the remnant lateral lower eyelid and the subsequent closure of the lid defect. This can also be performed with a lacrimal system reconstruction, when necessary, with a more physiological position.
Clinical cases
The MARCH technique has been successfully performed on multiple patients, demonstrating consistent outcomes and causing no significant complications. All patients were satisfied with the functional and cosmetic outcomes and the avoidance of two surgeries, or impairing other structures for the reconstruction.
Below are two cases highlighting the technique's ability to preserve the eyelid's function and maintain a natural eyelid appearance.
Patient 11 (Fig 1, see above) had a right lower lid basal cell carcinoma and required a tumour removal that left a defect of 75% of the lid length. Reconstruction using the MARCH technique included the use of a remnant lateral lower lid of 14% and an island pedicle flap. After one year, the patient remains stable without complications.
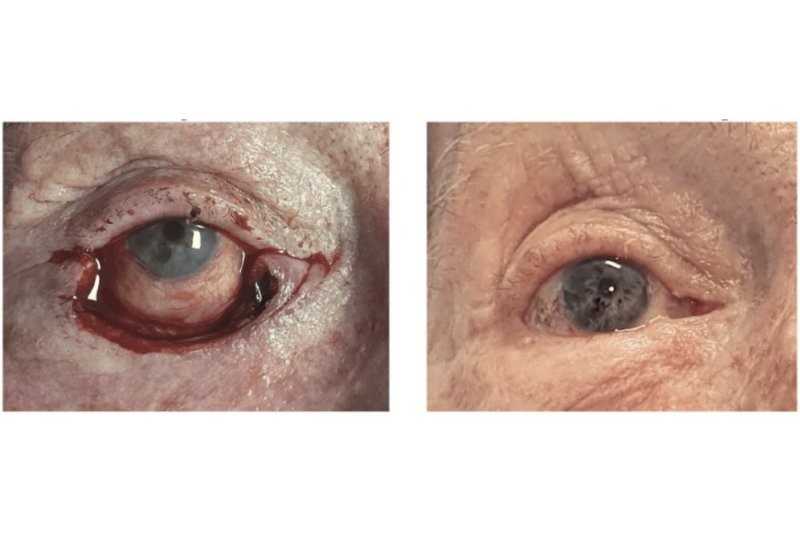
Patient 12 (Fig 2) was affected by a right lower lid basal cell carcinoma, underwent tumour removal and presented a secondary defect of the inferior canaliculus and the inferior eyelid of 79%. The reconstruction was achieved by the MARCH technique using an island pedicle flap and the implantation of a monocanalicular stent to repair the inferior canaliculus. Twenty-one months after surgery, the patient remains stable without complications.
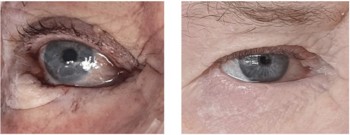
Fig 2. Patient 12, with intrasurgical defect (L) and at 20.9 months follow-up
Discussion
The MARCH technique offers several advantages over other reconstructive methods. One of the main benefits is that this does not sacrifice any other tissue apart from the lower eyelid which is already damaged. In the event of a recurrence, or a new tumour affecting the same lower eyelid, other procedures, such as a Tenzel flap, can still be performed afterwards. Thus, employing the MARCH technique as a first-line option preserves a wider range of future surgical reconstructive techniques.
Another important advantage is the MARCH technique is the only single-stage approach described for reconstructing lower eyelid defects exceeding 70% of the eyelid length. This avoids the need to keep the eye closed for several weeks and the necessity for a second procedure to open the eye, as required in the Hughes technique. This reduces the number of follow-up visits required, the cost of a second operation and the time that the patient is on sick leave. In addition, this procedure can achieve a better cosmetic result, allow the reconstruction of the lacrimal punctum in a more physiological position and preserve eyelashes in specific areas to maintain their physiological protection role for the cornea.
Nonetheless, beyond reconstructive techniques, skin cancer prevention remains essential. Patients should be reminded of the importance of preventing sun damage to the skin by walking in the shade, wearing protective clothing (such as long sleeves, collars, hats, sunglasses and umbrellas), avoiding peak sun hours, applying broad-spectrum, water-resistant sunscreen and seeking an early check-up when a suspicious skin lesion is detected. Through a combination of preventive strategies and advancements in reconstructive techniques, we can better support our patients.
Reference

Dr Anna March de Ribot is a consultant ophthalmologist specialising in oculoplastics with a particular interest in clinical research. She’s based at Whangarei Hospital and collaborates with Te Whatu Ora Auckland.