A trial fitting of RGP lenses for keratoconus
My journey with rigid gas-permeable (RGP) lenses has been one of self-discovery, particularly in this remarkable era of technology that allows me to capture and share insights instantly on platforms such as LinkedIn and Instagram. Screen sharing, topographies and various imaging tools, including EyeSpace and slit-lamp cameras, have transformed how we design lenses. Collaborating over the phone has become second nature, often relying on cellphone images – augmented with a Wratten filter – to empirically design lenses from our initial trials, with guidance from experts like Corneal Lens Corporation (CLC) director Graeme Curtis.
As most contact lens practitioners will attest, seeing lenses on patients is vital for understanding their performance, but collaborating with manufacturers and attending workshops such as the Cornea and Contact Lens Society (CCLS) or the Orthokeratology Society of Oceania (OSO) are invaluable for accelerated learning. I have been fortunate to glean insights from industry leaders like Hastings’ Tim Eagle, Hamilton’s Jagrut Lallu, Melbourne-based Shonit Jagmohan, Tauranga’s Alex Petty and, of course, director of EyeSpace in Christchurch, Charl Laas.
The case
A patient visited our practice in April 2015 with a history of RGP lens wear and established keratoconus. Initial assessments revealed unaided visual acuity of 6/48 in both eyes, with best corrected vision only achieving 6/24 in each eye. After a preliminary fitting with Rose K2 and Menicon sets, standard-edge lenses were fitted by September, achieving 6/7 vision.
However, in June 2023 the patient returned, reporting issues with the lenses flicking out. While the initial Rose K2 lenses allowed for reasonable vision correction (RE 6/7.5 and LE 6/20; unaided vision had dropped to 6/120), the fit needed improvement, prompting us to explore an asymmetrical corneal technology (ACT) design.


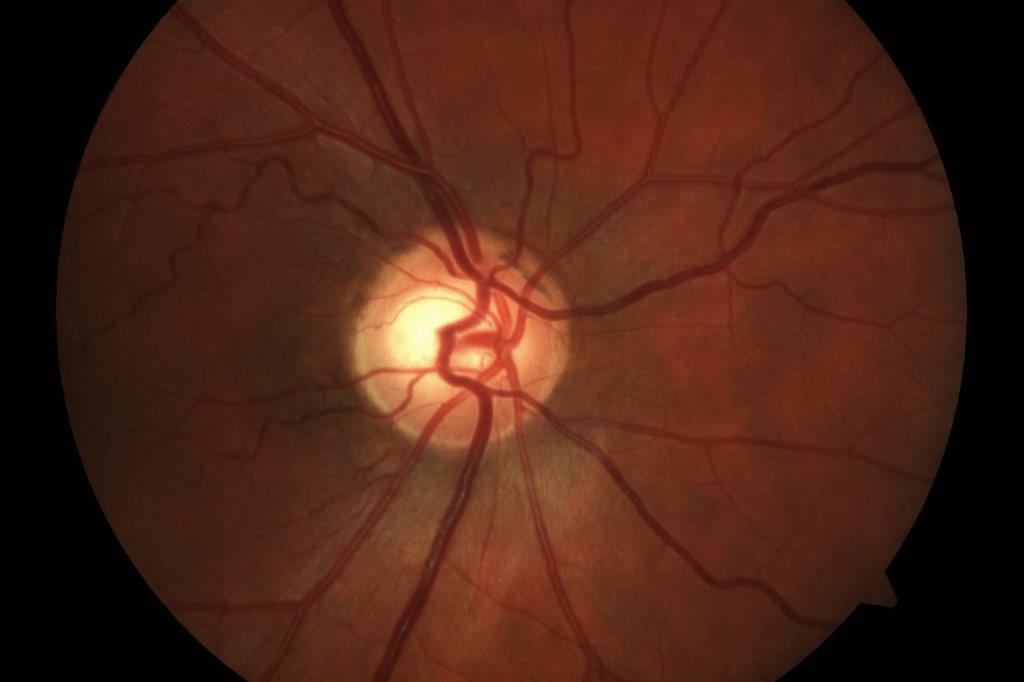
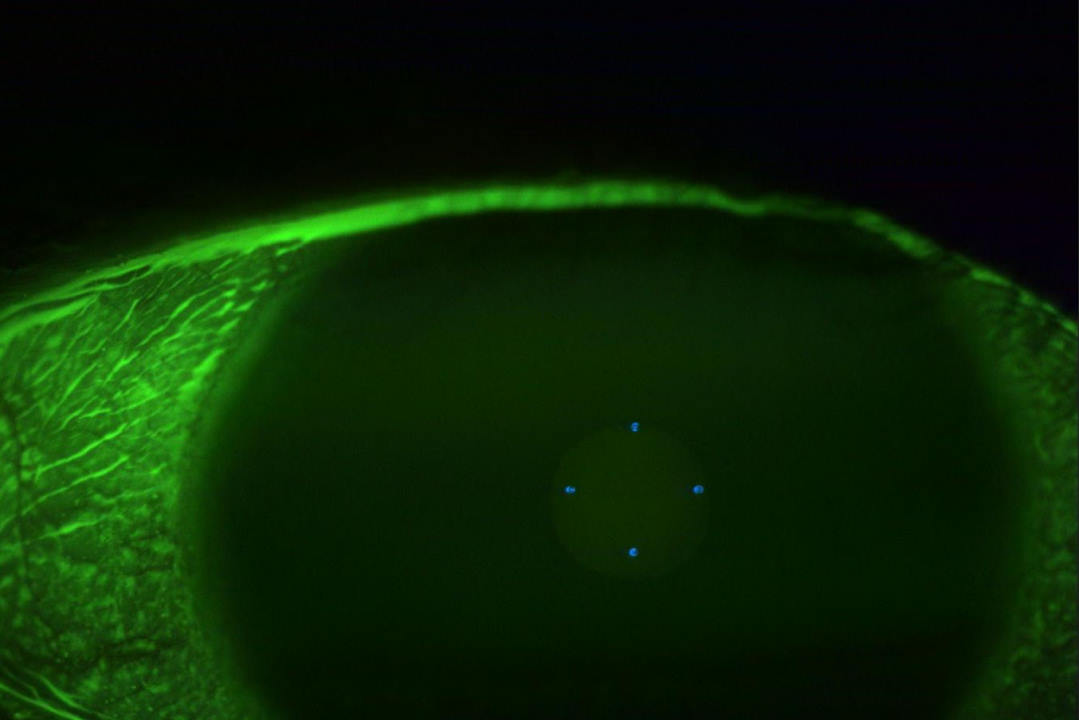
Figs 1A and B. BiSym RE and LE
During the refit, we had first tried adjusting the edge lifts in all four quadrants, but this had the RE lens sitting a bit flat and both sitting low with excessive edge lift. After switching to the quad sym design, the newly fitted lenses provided a better edge shape. Despite a two-week aftercare being booked, we didn't see the patient until the following April – after they had slept in the lenses and lost them.


Figs 2A and B. Nipple cone trials, RE and LE
Replacement quad sym lenses were ordered and another fitting arranged. Discussions with Alan Benjamin at CLC led us to try a Rose K2 nipple cone, resulting in a customised fitting that involved trialing a variety of lenses from the range. After some adjustments, including reductions in edge lift and incorporating a toric secondary and peripheral curve (TSP) to account for large inferior pooling, a new design was ordered.
The patient finally returned in July to collect his nipple cone lenses. Despite some faint staining from previous lens wear, the fit was stable, demonstrating an impressive flow of fluorescein and the lens sitting stable when transitioning between different gazes.


Figs 3A and B. Final nipple cone delivery, RE and LE
This case demonstrates the complexities of keratoconus fitting but highlights the fantastic vision an RGP can provide. It also shows how helpful the advancements in RGP lens fitting technology have become and the importance of strong communication with patients to reduce their time burden and encouraging them to attend fitting and aftercare appointments to get the best possible results.
For now, this patient has found success, and is comfortable, with stabilised lenses which enrich their day-to-day experience. The journey of lens fitting continues to be as much about collaboration and learning as it is about finding the right solution for everyone.

Ryan O’Connor is an optometrist and the director of Ashburton Eyecare. His specialties include myopia control, dry eye, therapeutics and foreign body removal and he has a passion for neuroscience, behavioural optometry and nutrition to aid patients with diabetes.