Case study: visual recovery after decompression
Case 1
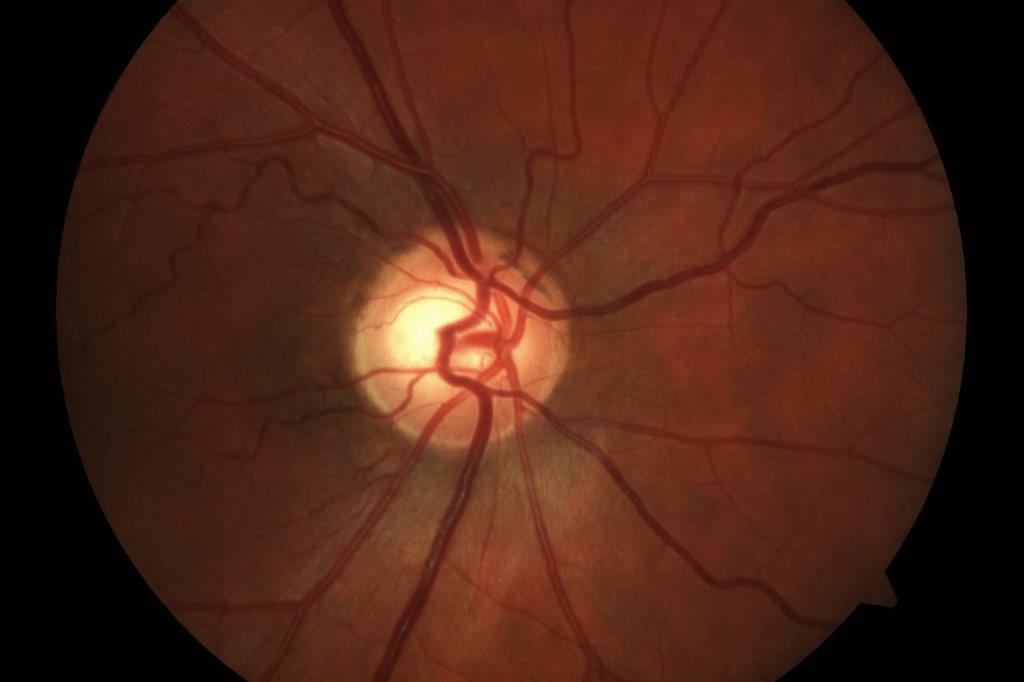
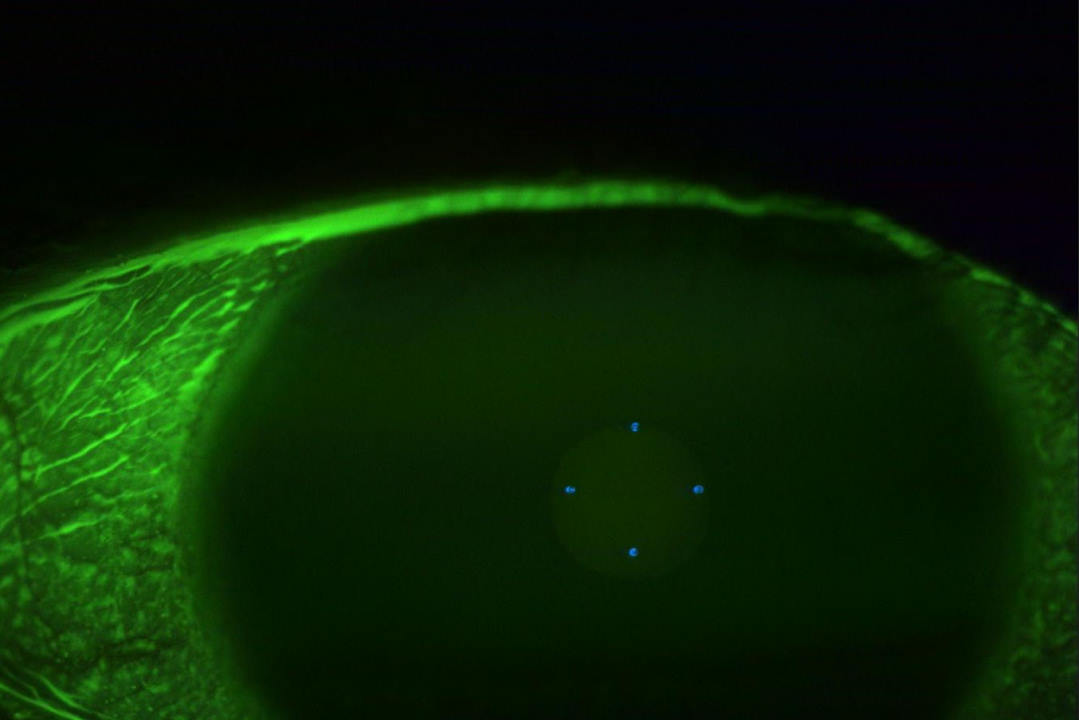
A 48-year-old man was referred with a diagnosis of normal tension glaucoma (NTG). He had a family history of glaucoma and was treated for systemic hypertension. Visual acuity was 6/6 in each eye, intraocular pressures were 17 and 18mmHg and central corneal thickness was 524 and 520µm. The optic disc assessment of the right and left eye showed a 0.65 and 0.5 cup-disc ratio, respectively, with possible neuroretinal rim thinning. The right Humphrey visual field (HVF) demonstrated a visual field defect consistent with glaucoma, while the left eye was normal. The right eye retinal nerve fibre layer (RNFL) showed borderline thinning in the temporal quadrant, while the left eye RNFL was normal.

Case 1’s visual fields over time. Visual field sensitivity improved at 18 months post-surgery
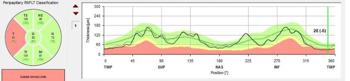
Case 1’s OCT of the RNFL
A closer examination of the right optic disc revealed temporal pallor. An MRI demonstrated pituitary macroadenoma with compression of the optic chiasm. The visual field gradually improved following the transsphenoidal resection of the pituitary adenoma. Optical coherence tomography (OCT) of the RNFL and ganglion cell layer remained unchanged.
Case 2
A 56-year-old woman referred for optic disc pallor had vision recorded as 6/6 in both eyes. HVF revealed an altitudinal visual field defect. The optic disc showed pallor. Her medical history included chronic hypertension. An MRI with contrast revealed sphenoid wing meningioma with optic nerve compression. It was considered inoperable. She underwent radiotherapy and the visual field defect improved gradually over the next few years. There was also some minor ganglion cell layer thinning in more recent examinations.

Case 2’s OCT RNFL thickness changes and visual field changes from 2021–2023; before treatment and two years after treatment. RNFL thickness decreased to 81μm; however, visual field defect improved
Discussion
Compressive optic neuropathy results from a lesion pressing on the optic nerve, resulting in optic neuropathy. If it is decompressed early enough, before the onset of optic atrophy, there is almost always some recovery1. OCT of the retinal nerve fibre layer and the ganglion cell layer is a good indicator of the recovery following decompression2. Some studies have shown that an average RNFL of more than 80µm pre-operatively predicts a good recovery3,4. Case 1 had an average RNFL thickness of 83µm and case 2 had 99µm. Similarly, the presence of a healthy ganglion cell layer thickness is a good predictor of recovery2. Despite minor ganglion cell layer thinning in case 2, the RNFL was preserved, which resulted in a good visual prognosis. On the other hand, visual field assessment and the visual field defect are poor predictors of recovery, as demonstrated in these cases.
Visual recovery occurs in three phases following decompression:
- Rapid recovery phase: this occurs within minutes to hours of decompression. It is likened to the relief of the conduction block after an arm ‘goes to sleep’5
- Delayed recovery phase: this lasts weeks to months and is related to the progressive remyelination of the previously compressed demyelinated axons5
- Late recovery phase: this lasts months to years and is slow. The exact mechanism is unknown.
Learning points
- Compressive lesions can vary in location and produce varying degrees of visual field defect
- There is almost always some recovery of visual field defect, but the extent of the recovery depends on the severity of compressive optic atrophy
- An MRI scan with contrast is invaluable in diagnosing intracranial or intra-orbital lesions.
References
1. Carlson AP, Stippler M, Myers O. Predictive factors for vision recovery after optic nerve decompression for chronic compressive neuropathy: systematic review and meta-analysis. Journal of Neurological Surgery Part B: Skull Base. 2013;74(01):020-38.
2. Garcia T, Sanchez S, Litré CF, Radoi C, Delemer B, Rousseaux P, et al. Prognostic value of retinal nerve fiber layer thickness for postoperative peripheral visual field recovery in optic chiasm compression. Journal of neurosurgery. 2014;121(1):165-9.
3. Danesh-Meyer HV, Papchenko T, Savino PJ, Law A, Evans J, Gamble GD. In vivo retinal nerve fiber layer thickness measured by optical coherence tomography predicts visual recovery after surgery for parachiasmal tumors. Investigative ophthalmology & visual science. 2008;49(5):1879-85.
4. Danesh-Meyer H, Papenchenko T, Law A, Gamble G. Pre-Operative Retinal Nerve Fiber Layer Thickness Correlates With Degree of Visual Recovery Following Surgery in Patients With Compressive Optic Neuropathy. Investigative Ophthalmology & Visual Science. 2007;48(13):2478.
5. Danesh-Meyer HV, Carroll SC, Foroozan R, Savino PJ, Fan J, Jiang Y, et al. Relationship between retinal nerve fiber layer and visual field sensitivity as measured by optical coherence tomography in chiasmal compression. Investigative ophthalmology & visual science. 2006;47(11):4827-35.

Dr Arvind Gupta is a consultant ophthalmologist based at Auckland’s Manukau Super Clinic, Greenlane Clinical Centre and Eye Doctors in Auckland, specialising in in cataract, medical retina and neuro-ophthalmology.

Kenny Wu is an Eye Institute and Te Whatu Ora Counties Manukau therapeutic optometrist with a clinical background in ocular surface disease and medical retina.