EI’s Sunday morning of eyecare pearls
Driving into the Aotea Centre early on an almost-summer Sunday morning felt a bit odd – not quite ready for work but not quite in relaxed weekend mode either. The unusual lack of traffic was noted, as was the normal plethora of roadworks, for those unaccustomed to driving in Auckland’s CBD. Greeted with breakfast, plenty of coffee and collegial chatter, the Eye Institute (EI) Annual Conference 2024 soon got underway featuring a line-up of 10 speakers.
Welcoming everyone, MC for the day Dr Narme Deva, admitted gathering so many doctors together on one day was like herding cats, particularly retinal specialists with extra talents such as ambidextrous surgeon Dr Will Cunningham, Dr Peter Hadden and his penguin patients, and a couple of movie-star doctors – Dr Sophie Hill, once an extra in a romcom, and Dr Kevin Dunne who’s appeared in a Japanese commercial!

Teresa Flanagan, Selina Phuah, Sheila Sim, Lizette Jordaan and Kerensa McCamis
The conference was divided into three sections, one focusing on the retina, another on glaucoma and the last on a few other areas the doctors wished to discuss. Each section was followed by 10 minutes of question time, which produced some of the best pearls of the morning. It was impressive how much each of the speakers shoehorned into their 15-minute slots, given the plethora of acronyms and slides.
Pachychoroid disease, retinal detachments on the rise?
Pachychoroid disease spectrum is a new term that appears to be flavour of the month, according to several optometrists who attended the most recent New Zealand Association of Optometrists conference. It describes a range of conditions related to attenuation of the choriocapillaris overlying dilated choroidal veins, and associated with progressive retinal pigment epithelium (RPE) dysfunction and neovascularisation. Dr Hill defined it as “characteristic anatomical and functional alterations of the choroid, including increased choroidal thickness and/or increased choroidal hyperpermeability”.


Keith Miller and Dr Phil Turnbull Amy Wang, Ice Liu and Alcon’s
Tristan Tuhi
At least six acronyms associated with pachychoroidal problems have been revealed and described since OCT became more advanced and more accessible in community optometry. Who knew there was so much to talk about in the choroid? Optometrists now need to take note of pachychoroidal changes and be able to identify which need referral for possible treatment or monitoring.
A recently identified pathology, focal choroidal excavation, is also getting picked up and referred more often due to increased OCT use. It’s usually only in one eye, often a myopic eye where there appears to be a backward dipping of the RPE with slight mottled appearance. Although the patient is usually asymptomatic, this finding warrants investigation as, occasionally, there can be leakage of sub-retinal fluid that requires treatment.
After giving us a thumbnail history of retinal detachment detection and repair, which was both amusing and horrifying, Dr Hadden went on to report that at least 5–10 people per 100,000 are treated annually for a retinal detachment in New Zealand. Many of these people will become bilateral and go blind if untreated. The retinal detachment rate may increase as more people become myopic, he said, but fortunately this is partially balanced by fewer cataract surgery complications.
Most retinal tears are caused by vitreous traction and are preceded by the classic ‘flashes and floaters’ symptoms. Most significant are Moore’s lightning streaks, which are temporal, white lightning-like and more noticeable in the dark or on head movement.


Michele Foster, Vandana Kumar, Brian Appleyard, Stephen Hill
Vicky Wang and Jas Walia and Gary Filer
Addressing vitreous traction holes using vitrectomy and gas bubble has the advantage of getting rid of the traction and sealing the hole with less consequent refractive change and discomfort. According to Dr Hadden, the surgeon gets a better view of the hole, is also able to seal smaller and more posterior breaks in the retina and can use long-acting oil tamponades. The downside of this method is the expansile gas can actually cause holes as it expands! The patient is unable to travel by air and the likelihood of developing a nuclear cataract is increased, probably due to more oxygen getting into the lens. Approximately 25% will get a detachment in the other eye, therefore flashes and floaters should be seen to promptly.
The dreaded crunch syndrome
We thought Dr Dunne was joking when he started his talk about “the feared crunch syndrome”, aka the medical retina specialist’s fear of Avastin (bevacizumab). Crunch syndrome in progressive diabetic retinopathy (DR) refers to the increased risk of tractional retinal detachment after the use of anti-VEGF treatment. The incidence quoted in the literature varies from 1.5–18.4%, but is generally at the lower end, now more is known about the risks.
Progressive DR leads to increased permeability and ischaemia, an increased risk of diabetic macula oedema (DMO), an increase in vascular endothelial growth and subsequent proliferative DR (PDR). The natural history of untreated PDR is new vessels appearing at the disc, iris and angle, with consequential risk of vitreous haemorrhage, tractional retinal detachment and/or neovascular glaucoma. Anti-VEGF injections not only treat DMO, but may also help control PDR, hence performing a dual role. Traction of any form potentially causes retinal detachment.
Retrospective studies have shown the timing of anti-VEGF crunch typically occurs one to six weeks after injection and the pooled analysis did not support the hypothesis that anti-VEGF increased the risk of tractional retinal detachment in PDR. However, there are risk factors including the presence of a ring-shaped fibrovascular membrane, higher dose of Avastin (typically higher than used in New Zealand), having diabetes for more than 15 years, more than a 12-day delay from injection to a vitrectomy procedure and untreated or severe PDR with fibrosis.
From the optometrist’s point of view, the message is to be aware of what is happening to long-term diabetic patients, liaise closely with their vitreoretinal specialists (if that’s possible), giving as much detail of history as you can… and mind the crunch!
On the other hand…
Dr Cunningham clarified that he is not actually a closet ambidextrous surgeon, but a left-hander taught by right-handed surgeons, before posing the question of whether or not dietary supplements break up vitreous floaters and make them disappear. In a recent double-blind study of 61 patients, it was reported 77% on the active supplement VitroCap N demonstrated a reduction in vitreous floaters, with 67% of these patients reporting an improvement in quality of life.


Drs Graham Reeves and Eva Woodward, Tiffany Ong and
Will Cunningham Evelyn Tee
Dr Cunningham then discussed some vexing questions, such as “when is a macular hole not a macular hole?”. The answer to this one was: when it has gone away spontaneously. Likewise, can a retinal detachment, which has been present for a while that’s showing pigment changes and is peripheral and asymptomatic, be monitored? OCT is needed to confirm if it is a detachment or retinoschisis with no obvious break. For the optometrist, even with a fancy OCT, when in doubt refer and let the retinal surgeons make the decision. As my kids would say: “That’s above my pay grade!”.
Those who find that horrible Shingrix advert disturbing would have definitely been rattled by Dr Jay Meyer’s presentation on herpes zoster ophthalmicus (HZO) – especially attendees over 65, the median age for developing shingles, or those knowing people over 85, who face a 50% risk of contracting shingles, with 9% experiencing recurrent episodes.
There is an increasing incidence of herpes zoster worldwide, which appears to be more prevalent in Caucasians than in Pacific Peoples, for reasons unknown. This may be a spurious result, as the studies are mainly from Hawaii, however, Pacific Peoples have a higher incidence of atopy, which is another risk factor for HZO. Another sobering fact is that 25% will have pain beyond three months, leading to high rates of depression; this is a common cause of suicide in people over 70 years of age. There is also an increased risk of stroke, heart attack, malignancy and giant cell arteritis.
Half of HZO patients will develop ocular involvement, and those with Hutchinson’s sign – a rash involving the tip of the nose – are twice as likely to be among them. The Zoster Eye Disease Study (ZEDS) trialled long-term antiviral treatment’s (valacyclovir) capacity to reduce the complications of HZO, including new or worsening chronic eye disease and post-herpetic neuralgia. The results showed no significant benefit at 12 months, but significant benefit at 18 months with shorter duration of pain and significantly less neuropathic pain medication required. Antivirals started within three days can also reduce the severity of symptoms.
A patient with HZO and minimal eye involvement can be checked by an optometrist but should be rechecked after one week because they can still develop iritis, so dilation and repeat monitoring is required, said Dr Meyer.


Navpreet Dhaliwal, Patrisha Bertulfo Anuja Malhotra, Harriet Pita and
and Kenny Jung Jacob Benefield
The new Shingrix vaccine is supposed to be over 90% effective – but for how long, we don’t know. The same was claimed for the older vaccine, Zostavax, which has since been shown to be only 50% effective. The total cost of vaccination is $700–$800 and is given in two injections several months apart. The vaccine is free for 65-year-olds and, since 1 July 2024, also fully funded for certain immunocompromised people over 18 years of age. It’s necessary to wait until the patient is totally recovered before vaccination, as the vaccine can exacerbate unresolved symptoms.
Benign, malignant or neither?
Optometrists should be viewing every eye from front to back, and the ‘funny spot’ on the lids always viewed with suspicion, said Dr Adam Watson. Asking “is it benign or malignant?” should be routine for optometrists, and the answer most likely depends on whether it’s “stuck on the surface” or has tentacles invading below the surface.
When there is central ulceration, eyelash loss and pearly edges, it’s concerning, especially if it is irregular in shape, possibly with blurred margins, inconsistent colour and/or thickness, asymmetric and appears to be growing. So push the referral button and let an ophthalmologist take a look at it, he advised.
On another note, those nasty little transparent crawly things that look like crabs clinging to the eyelashes in clumps when viewed under the slit lamp, are actually lice (not the demodex mite), and may need immediate attention. They can be picked off with forceps, Dr Watson said, but that’s inadvisable if you are already running late and have a full waiting room! Drowning them in an oily ointment has been known to slow them down, or you can recommend the patient tries permethrin 1% shampoo and has a chat with their GP about contact tracing and lifestyle changes. In my experience – once the cause of the incredibly itchy eyes is tactfully revealed – my examination chair is speedily vacated.
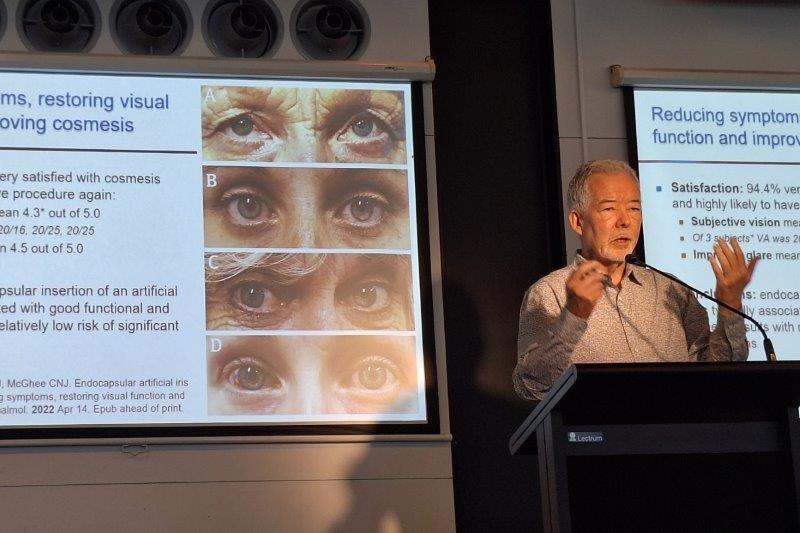
Dysphotopsia – often seen, rarely understood
Dysphotopsias are a common source of dissatisfaction post-cataract surgery, said Dr Shanu Subbiah. They are unwanted visual phenomena from external light sources causing light to enter the eyes and impacting the retinal image by causing shadows and patterns. Typically they are transient, settle within weeks or months and are more likely to occur with multifocal or extended-focus intraocular lenses (IOLs). There are two types of dysphotopsias: positive and negative.

Kathryn Sands, Bhavna Patel and Sachi Rathod
Positive dysphotopsias are bright artefacts of light on the retina causing glare, flickering, shimmering or haloes of light in the peripheral vision. These are never seen in the dark, only in light or half-light conditions. Up to 70% of patients notice them soon after cataract surgery, reducing to less than 20% after one year. The cause may be related to trauma during surgery or to the IOL’s curvature, diameter or lens material. Other causes include pupil size or residual refractive error. The management of positive dysphotopsia may include use of miotics, but YAG laser capsulotomy is definitely not advisable. If all else fails, exchanging for an IOL made with a different material or design may have to be considered.
Negative dysphotopsias are less well tolerated. They are seen as temporal, arc-shaped shadows in a normal visual field and may be related to shallow orbit and prominent globe, allowing more incident temporal light to fall onto the nasal retina. Other possible origins include IOL centration, smaller pupils or high-power IOLs. There is likely to be a neuroadaptive component – a nice way of saying the patient will get used to it eventually – and the proof is in the reduced awareness over time. However, this diagnosis has to be treated with caution until all other possibilities – such as retinal detachment, posterior capsular opacification or striae, posterior vitreous detachment, entoptic phenomena such as phosphenes, or optic neuropathy – are discounted. Explaining pre-operatively that dysphotopsia is common but becomes less noticeable with time helps reduce anxiety and manage expectations, said Dr Subbiah.
The overall theme of this year’s conference appeared to be on issues that may be observed but not always recognised. While giving up half a Sunday is tough after a long week, the opportunity for total immersion in continuing education and adding to our CPD tally in a single hit without distraction was welcome. It certainly got a big thumbs up for format and content from those around the lunch table.

Naomi Meltzer is an optometrist who runs an independent practice specialising in low-vision consultancy. She is a regular contributor to NZ Optics.